국제환자진료
Thyroid Radiofrequency Ablation (RFA)
Thyroid RFA is a non-surgical treatment of benign symptomatic thyroid nodules remaining no incision nor scar. Not need to take medicine after treatment.
What is thyroid RFA?
Thyroid RFA is a non-surgical treatment for large symptomatic thyroid nodules by radiofrequency induced heat. In the past, large nodules were treated with surgery, even if they are not cancers. Thyroid RFA is a non-surgical alternative to treating large benign nodules avoiding surgery.
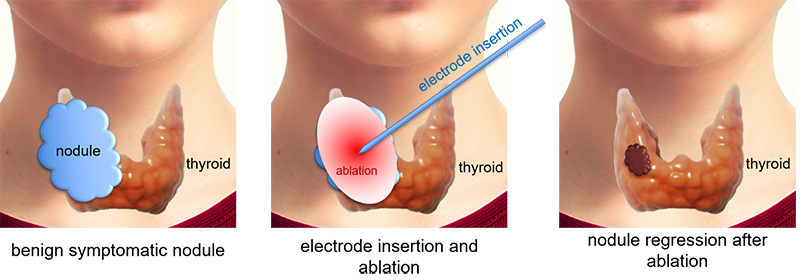
Figures: Insert an RFA electrode, which looks like a needle, about 1 mm thick, into the nodule under the ultrasonography guidance. Ablate the nodule with the heat generated from the electrode. Thermally ablated nodule tissue is absorbed into the patients' body over time.
Thyroid RFA started to operate primarily to treat benign nodules as it is widely used to treat recurrent thyroid cancer. Nowadays, it is currently under investment to treat small low-risk papillary thyroid cancer.
Basic principles of thyroid RFA
Concretely speaking, the RFA procedure is not so fantastic, as illustrated in the figure above. For the successful RFA, the following three factors are required.
1. The procedure should be done very carefully little by little until the entire volume of the nodule is ablated.
2. The thermal energy of RFA should not be spread beyond the nodule to prevent complications
3. The larger the nodules, the more strategically planned the treatment should be.
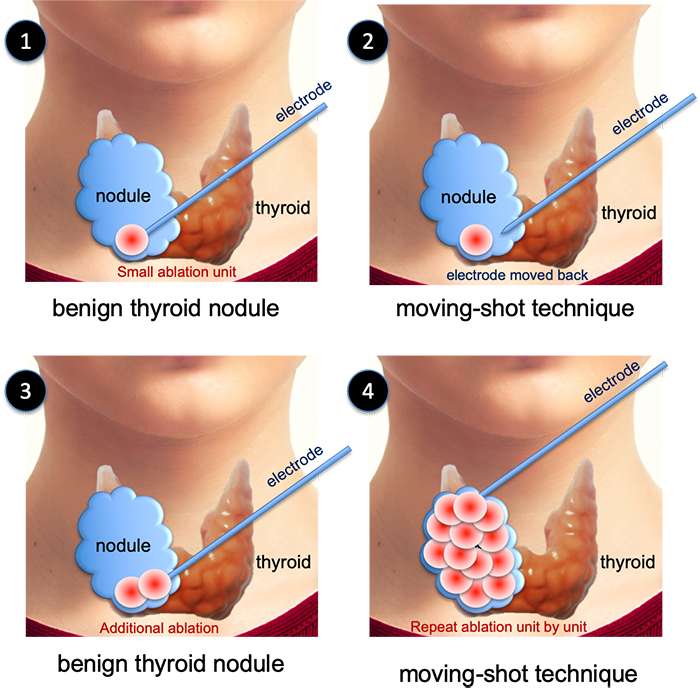
1. Moving-shot technique: the principle of ablating little by little
RFA is usually done for large nodules. When we treat large nodules with RFA, we ablate gradually unit by unit, starting from one corner. Under the ultrasonography guidance, an RFA electrode is inserted into the outer and lower corner of the nodules and then ablation proceeds for the very unit (Figure ① below). Then the electrode is withdrawn little (figure ② below). Another ablation is made (figure ③ below). In this way, a small ablation is repeatedly proceeded to ablate the entire nodule (figure 4 below). This method is called the moving-shot technique. The technique is introduced by Professor Jung Hwan Baek for the first time, at Asan Medical Center in Seoul.
2. The thermal energy of RFA should not be spread beyond the nodule to prevent complications
Even if we do the best treatment using the moving-shot technique, the outermost part should be left untreated. (Figure ④ in the above shows that the outermost part remains untreated) Leaving the marginal area untreated is not because we can't ablate there but attempting to ablate marginal tissues brings a risky result of thermal damage development to adjacent normal tissues. Nodule tissue should be ablated, but the normal peripheral structures should not be thermally damaged. In the neck, where there are a lot of critical structures are in a tight space, special care must be enacted to avoid damage.
3. The larger the nodules, the more strategically planned the treatment should be.
Even with the best use of the moving-shot technique, very thin nodule tissue is left at the margin, the remained amount of tissue is rather a lot than we may think.

This figure illustrates that the very thin tissue still stays at the margin as we’ve done the moving-shot technique excellently. As you can see on the very left conceptual diagram, the moving-shot technique is well applicated and only a thin layer of nodule tissue has remained. It seems like the nodules are completely ablated. For your better understanding, please refer to the second photo above. I cut a thinly peeled tangerine in half. As I mentioned, the peel is very thin. RFA procedure is similar to ablate the flesh of tangerine and leave the peel. In the second photo, the peel seems very thin and has only a small volume. However, as you can see in the third picture, the volume of the peel is quite larger than we imagined when it’s fully peeled off and collected. Through these figures, we could understand that the volume of remaining marginal nodule tissue is comparably large even with the very good use of the moving-shot technique.
The larger the nodules with large initial volume, the stronger the tendency it has to recover to their original volume though the reduction was achieved with ablation. As a result, the remaining tissue may grow again. Therefore, the remaining tissue after the first treatment should be ablated again for adequately selected cases.
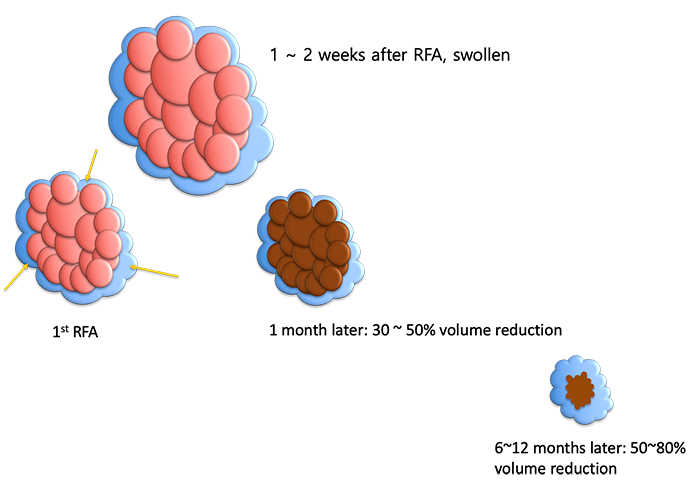
Nodules are swollen for 1-2 weeks after the RFA, so the volume becomes larger than before treatment. But, after about a month, the volume decreases by 30-50%. Therefore, about a month after the first treatment, patients usually feel symptoms have been improved. After RFA, nodular tissue is absorbed gradually over six to twelve months. The usual volume reduction is 50% to 80%.
However, even with the improved symptoms, the larger the volume of nodules before treatment, the greater the amount of tissue remaining after treatment. If patients misunderstand about this condition; the complete resolution is yet to be done and left the nodule without adequate treatment afterward, the remaining nodule tissue can grow again. Therefore, it is important to take appropriate additional treatments at this point until it’s resolved completely.
In general, averagely three treatments are required to treat the 4cm nodule completely. If you are lucky, it would end once or twice, but if the location is not convenient, or there is a lot of blood supply from the nodule, the number of RFA session may increase.
Comparison between RFA and Thyroid Surgery
Strength of surgery and disadvantage of RFA
The advantage of surgery is that all problems can be solved by one-time treatment under general anesthesia. Surgery of a benign tumor also has little recurrence chance; so a single operation means cure itself. Unlike RFA, it can be done after a single FNA / core needle biopsy. Indeterminate nodules, such as atypia or follicular neoplasm, can also be treated with surgery as well as got final diagnosis.
The most prominent drawback of RFA is multiple treatments are required for large nodules, instead of single definitive treatment explained above. Another disadvantage is the necessity of two times of FNA / core needle biopsy: and only available for definitively benign nodules.
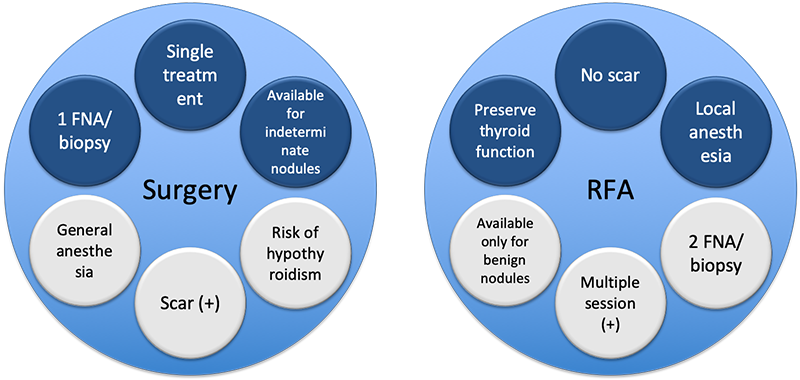
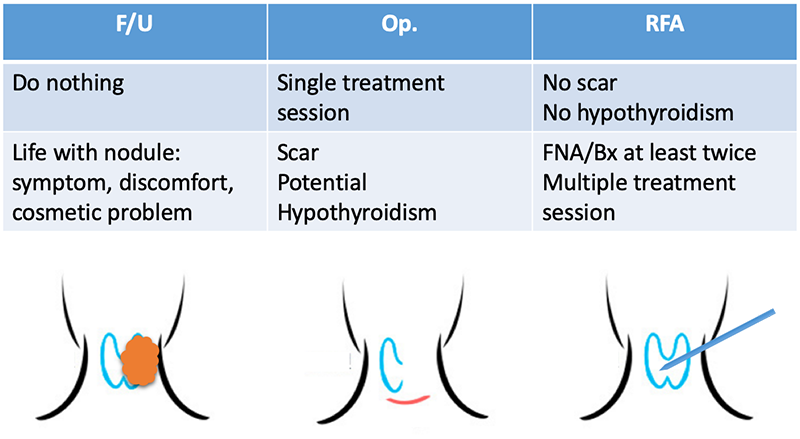
RFA remains no scar, because this technique uses very thin, needle-like a shaped electrode. Surgery leaves a scar, however, recently introduced endoscopic and robotic techniques leave it in other sites than the easily visible neck, such as axillary, nipple-areolar, or oral mucosa.
RFA treats only nodules preserving thyroid tissue. Surgery sacrifices at least half of the thyroid. About 1/3 or 1/4 of patients suffer from hypothyroidism and ingest thyroid medicine for the rest of their lives after surgery.
RFA is done under local anesthesia, leading to early discharge from the clinic, usually within 2 to 6 hours after the procedure. Surgery requires general anesthesia and a few days of hospitalization.
Frequently Asked Questions on RFA
1. Do they do general anesthesia to do RFA?
No. RFA is performed with local anesthesia on the skin and tissues around the thyroid gland. This is because the pain is not so severe as to require general anesthesia, and there is another important reason to use local anesthesia. The two most common complications that can occur during the RFA are heat damage to the nerves for voice production and the blinking. Therefore, during the RFA, the operator asks the patient to speak something or blink. However, general anesthesia cannot make this kind of confirmation.
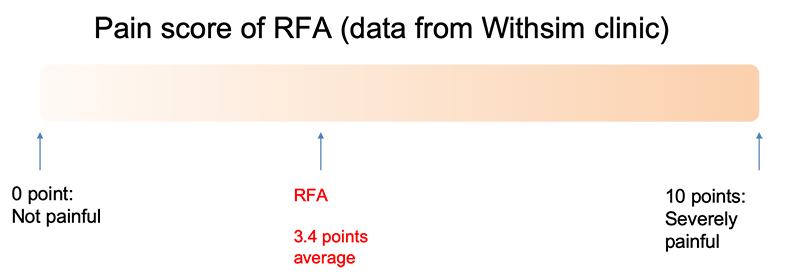
2. How painful is RFA?
It is not so much painful. Assuming the severe pain is 10 points, and no pain is 0 point, the patients marked 3.4 points when they’re asked about the degree of pain after RFA. Most of the time, they said "somewhat painful but tolerable.”
3. How long does it take to do RFA?
The net procedure time for RFA is about 10 minutes for nodules around 3cm, and 30~40 minutes for 5 or 6cm. If we include preparing time and post-procedure caring time, it is about an hour. After the procedure, 2 to 6 hours of resting and observation is needed to check whether there is severe swelling or uncontrollable bleeding.
4. What is the indication of RFA?
RFA is to do for the patients with a symptomatic benign thyroid nodule. Symptoms are mainly due to compression from nodule’s bulk, include dull pain, foreign body sensation, cough. etc.
5. Why at least two times of FNA or core needle biopsy are needed before RFA?
There are cases that are confirmed to be malignant after surgical excision, even though pre-operative FNA was benign. These cases are rare but important. It must be surprising for the patients, however, they can treat their malignant tumor in a proper way with a very high rate of complete recovery.
But if these kinds of false-negative nodules were treated with RFA, there would be no change to get the right diagnosis, for none of the tumor tissue is excised out. A part of these cases can recur as cancer.
Thus, benignity confirmation is much more important for RFA and surgery, which is the reason why at least twice of FNA or core needle biopsy is necessary. Moreover, the latest one should be done within one year.
The RFA guideline published by the Korean society of thyroid radiology in 2018 added new content that wasn’t on the previous 2013 version. One time of FNA or core needle biopsy is enough for the nodule having undisputedly benign ultrasonography findings. This is only when the expertized profession interpreted the ultrasonography.
6. Can I do RFA for an asymptomatic small nodule to avoid becoming cancer in the future?
Many patients ask to ablate asymptomatic benign nodules, only because they fear cancer. This is not an indication of RFA. If small nodules were diagnosed as benign, they are absolutely safe. Proper interpretation of the condition and counseling is enough for the patients’ safety and well-being.
7. Can I do RFA for nodules with atypical cells, follicular neoplasms and/or Hurthle cell neoplasms?
Leaving nodules with atypical cells or excising half of the thyroid with indeterminate neoplasms are both unfavorable. Many patients want to solve their clinical problem more confidentially and less invasively. However, RFA can not be a solution for those cases. Currently, RFA is advised for benign symptomatic nodules, recurrent thyroid cancers and selected cases of low-risk microcarcinomas. RFA for nodules with Indeterminate cells is not advised.
8. Is recurrence frequent after RFA?
We do not ablate all the tissue of nodules in a single session of RFA. Nodule tissue near the margin remains untreated. The large the nodule is, the larger the remaining vital tissue is. If we leave the remnant tissue untreated, it can regrow. Adequate follow-up surveillance and additional ablation are important not to regrow and recur.
9. Is RFA a multiple-session treatment?
Yes, it is. As answered in question 8. additional treatment is essential for some cases, especially when the volume before RFA was large. Small nodules around 3cm can be treated within a single session, but RFA for small nodules are usually not necessary because they do not cause symptomatic and/or cosmetic problems. Most of the nodules causing pressure-induced clinical problems are larger than 4cm, which is hard to complete treatment with a single session. Thus, it is important to approach strategically using well-planned multiple sessions of ablation.
10. How many times of RFA is needed to complete treatment?
The most important factor is the nodule volume before treatment. The table below shows the number of sessions according to initial nodule volume.
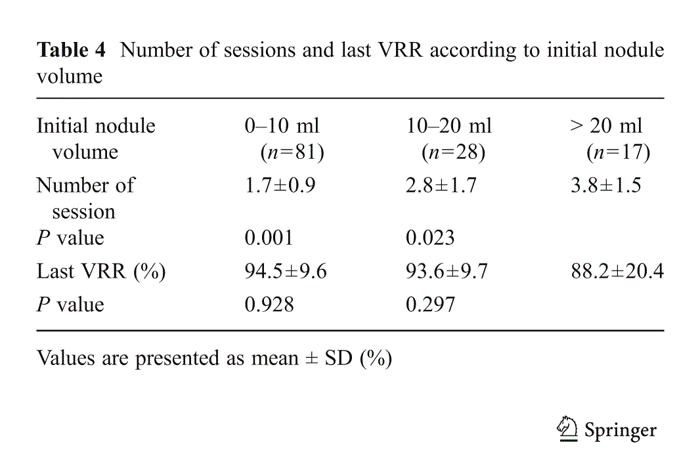
They did RFA 1.7 +/- 0.9 times for the nodules with 0 ~ 10mL of volume, 2.8 +/- 1.7 times for 10 ~ 20mL, and 3.8 +/- 1.5 times for 20 ~ mL. Ususally, a 10 mL nodule has 3 ~ 4cm length and a 20 mL nodule has about 5cm length.
This data was published in 2013. They did RFA 4 to 1 year prior to the publication. Nowadays the number of sessions has reduced by 2 to 3 times.
11. Can RFA treat papillary thyroid carcinoma?
It is promising but still under investigation.
Papillary thyroid carcinomas of which the length is less than 1cm are called papillary thyroid microcarcinoma (PTMC). Most of the PTMCs are not growing for some decades even if they are left untreated. They do not harm patients as well.
Some experts claimed that leaving PTMCs untreated is safer than doing surgery considering the basic operative mortality and morbidity. Their opinion was fairly proved by more than 30-year of observation. Now we call this kind of observation active surveillance. Many expertized institutions offer active surveillance as a standardized option for managing PTMCs.
Active surveillance is now accepted widely and long-term follow-up results are favorably accumulated. Researchers found only a few PTMCs are growing. Some of them suggested if PTMC were so stable, then why we don’t follow them after ablating with RFA. This concept is raised among pioneers around ten years ago and now is called RFA-assisted active surveillance. Earlier, they applied RFA-assisted active surveillance for the patients who were not eligible for surgery or general anesthesia and they reported the results were excellent. Now some advanced groups applied this technique for healthier patients.
China is the most active nation for RFA-assisted active surveillance. Years ago, they reported RFA is safe and effective for treating PTMC. However, the follow-up period was too short to be certain about the RFA only within 1 or 2 years period. But recently they published meaningful data for RFA-assisted active surveillance. I would like to introduce the most important 3 reports here below.
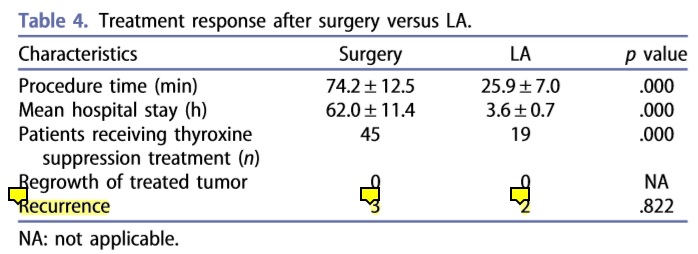
The first one is from Bejing in 2019. They follow up for 5 years, about half of them performed surgery and the others RFA-assisted active surveillance. Below is the most important table of the report.
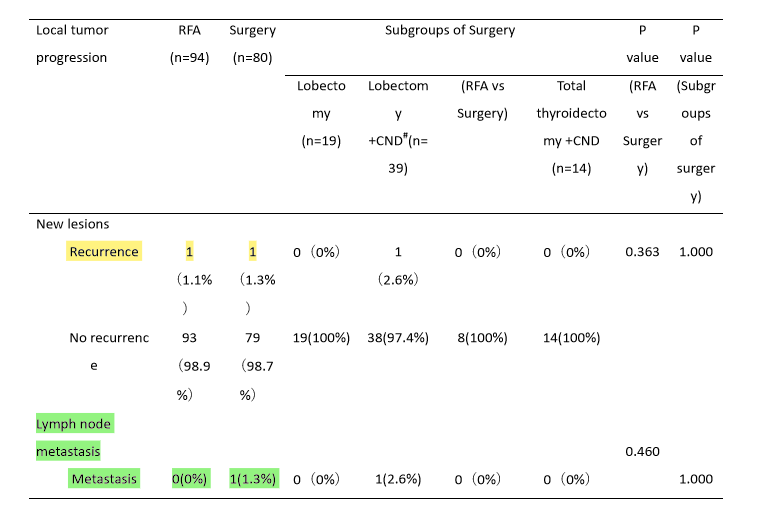
Yellow high light shows the recurrence number. Both RFA and surgery groups show 1 recurrence case. Green highlights show lymph node metastasis. No metastasis was found in RFA group while 1 metastasis was found in surgery groups. RFA group showed not inferior performance than surgery for 5 years.
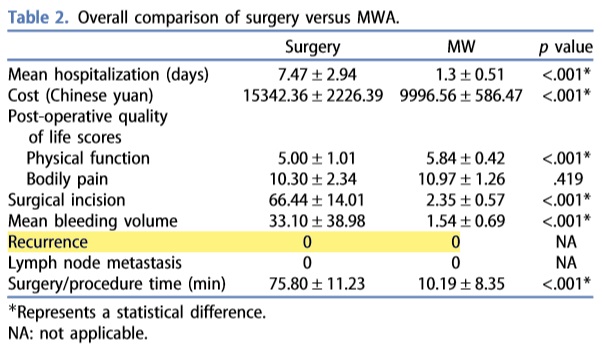
Two other researches show the equal performance of thermal ablations and surgery in terms of recurrence. In this researches, one of the authors used laser ablation (upper table), and the other authors used microwave ablation. Laser and microwave are basically the same as RFA, the only difference in the mechanism of forming thermal energy.
Now, we can expect the more active application of thermal ablation for treating PTMC with the accumulation of favorable data.
12. Can RFA treat recurrent papillary thyroid carcinoma?
RFA for recurrent thyroid carcinoma is prooved to be safe and effective for a long time.
We are good at Thyroid RFA.
We know well thyroid nodules and ultrasound.
We are studying, teaching and collaborating with the world.
Recent Publications related to Thyroid & Ultrasound from Withsim Clinic
Sim JS, Baek JH. Long-Term Outcomes Following Thermal Ablation of Benign Thyroid Nodules as an Alternative to Surgery: The Importance of Controlling Regrowth. Endocrinol Metab (Seoul). 2019 Jun;34(2):117-123.
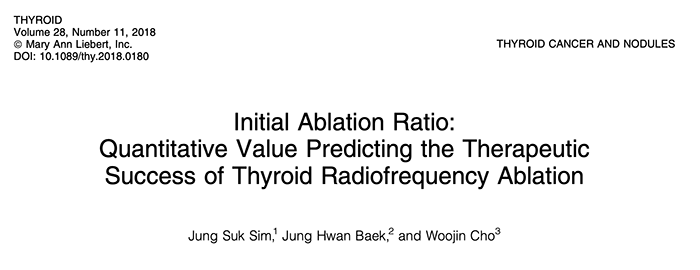
Sim JS, Baek JH, Cho W. Initial Ablation Ratio: Quantitative Value Predicting the Therapeutic Success of Thyroid Radiofrequency Ablation. Thyroid. 2018 Nov;28(11):1443-1449.
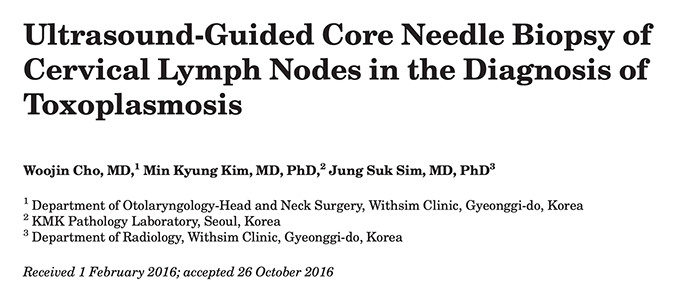
Cho W, Kim MK, Sim JS. Ultrasound-guided core needle biopsy of a cervical lymph node in the diagnosis of toxoplasmosis. J Clin Ultrasound. 2017 May;45(4):192-196.
Sim JS, Baek JH, Cho W, et al. Radiofrequency ablation of benign thyroid nodules: depicting an early sign of regrowth by calculating vital volume. Int J Hyperthermia. 2017 Apr 10:1-6.
Cho W, Lim DH, Park HC. Transoral sonographic diagnosis of submandibular duct calculi. J Clin Ultrasound. 2014 Feb;42(2):125-8
Cho W, Hong JH, Park HC. Real-time ultrasonographic assessment of true vocal length in professional singers. J Voice. 2012 Nov;26(6):819.e1-6.
Invited Speaker at...
2020 Spring Meeting of the American Thyroid Association®(ATA), New York, USA (2020)
Transoral Thyroidectomy Workshop of Chinese University of Hong Kong (2018, 2019, 2020)
9th International Robotic Surgery Symposium(IRSS), Seoul, Korea (2019)
17th World Federation for Ultrasound in Medicine and Biology Congress (WFUMB), Melbourne, Australia (2019)
The 42nd Japan Association of Breast and Thyroid Sonology, Tokyo, Japan (2019)
Congress of Asia-Pacific Society of Thyroid Surgery (2015, 2017, 2018)
A continuous Medical Training Program at Medical University Center Ho Chi Minh City, Vietnam; "RFA application for treatment of benign thyroid nodules"(2016)
2015年中国超声医师学术大会 (2015)
Head & Neck Ultrasound Workshop in 67th Annual General & Scientific Meeting of New Zealand Society of Otolaryngology Head & Neck Surgery, Rotorua, New Zealand (2014)
20th World Congress of the International Federation of Oto-Rhino-Laryngological Societies (IFOS), Seoul, Korea (2013)
Awards
Award for International Publication of the Year at Annual Congress of Korea Society of Medical Ultrasound (2019)
The First Prize : Best Presentation Award of The Year At Annual Congress of Korean Society of Otorhinolaryngologic Clinician (2017, 2012)
Best Thyroid Clinic of The Year from Korea Customer Appraisal (2016)
We’ve educated doctors from...
Brazil, Vietnam, China, Hong Kong, Mongolia
We’ve treated Patients from...
USA, Japan, Hong Kong, New Zealand, Chile, Germany, China, Canada, Vietnam, Mongolia